Are Bone Marrow Transplant Patients Immunocompromised - More BMT Truth Unveiled!
Are bone marrow transplant patients immunocompromised? A common question among people undergoing this treatment - it requires deep understanding of the condition and the treatment.
Also known as stem cell transplantation, BMT is a life-saving process for individuals with issues such as leukemia, multiple myeloma and lymphoma. This treatment offers a chance at a cure, but has significant risks for both parties.
The following sections look into the different issues people who have undergone BMT experience.
Why Do Some People Experience Severe Effects of BMT
The procedure carries significant risk, including immunosuppression and changes in blood type. However, their prevalence differs on the type of BMT the patient undergoes.
From Graft vs Host disease (GVHD) to immunosuppression, there are various repercussions of this treatment.
Such ill-effects are seen due to the altered immune system that the patient has after the transplant.
This is mainly due to the destruction and replacement of the stem cells. In addition, as the patient undergoes high-dose chemotherapy before the process to kill the cancer cell, it also ends up suppressing the immune system to prevent rejection of the donor cells.
This is one of the many reasons why people undergoing BMT (especially the recipient) develop poor symptoms. The following section explores the most prominent risks of the procedure for both recipient and donor.
Are Bone Marrow Transplant Patients Immunocompromised?
Yes, patients who undergo BMT become immunocompromised, this is mainly due to the high-dose chemotherapy before the procedure. This immunocompromised state develops due to the time lag in immune reconstitution.
This is the gap in the immune system to have its defense system up and running. This can be around weeks to months and years - and if during this gap the patient develops chronic GVHD, the immune recovery delays further.
This lag in restoration of the immune system leads to high risk of infections.
Best ways to handle this and prevent further deterioration of health:
-
Keep patients in isolation.
-
Provide prophylactic antibiotics.
-
IVIG - antibody infusions.
Why does blood type change after BMT?
The blood type is determined by the bone marrow, and a change in blood type is seen in allogeneic BMT. The plasma contains surface antigens A, B, and Rh and the plasma (clear liquid in the blood that you see when a wound starts healing) carries the antibodies against non-self blood types.
For example, if you have Type A blood (RBCs have A surface antigens), your plasma would have anti-B antibodies - antibodies against the B type surface antigens.
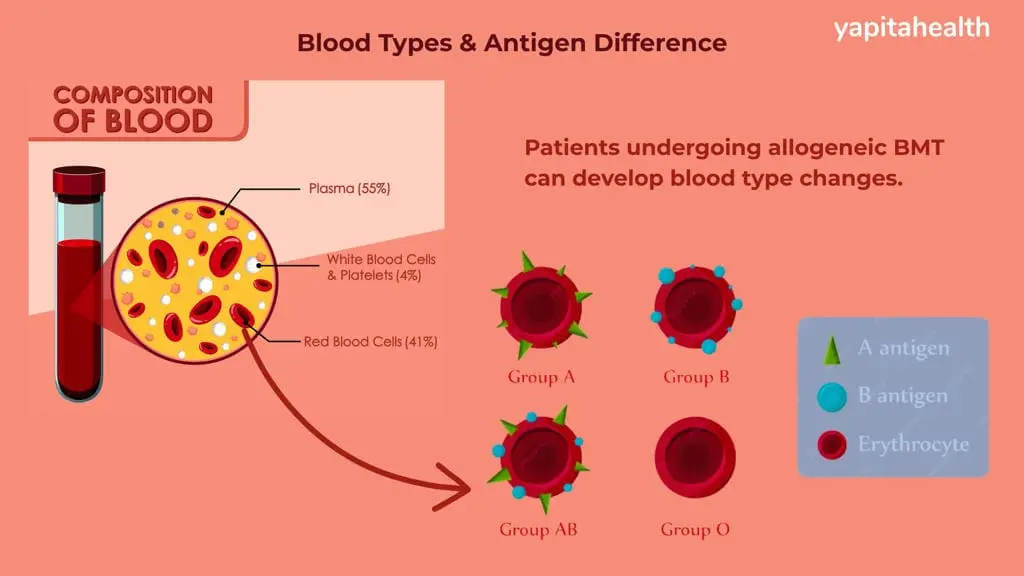
During BMT, the recipient’s own blood cells die off during chemotherapy which allows the donor’s stem cells to produce the new RBCs. The old plasma antibodies fade within 3-6 months.
Thus, autologous BMT does not lead to a change in the blood type. Consider this example -
-
If the donor has type O blood and the recipient has a type A blood, it can take a period of weeks to months post-transplant for the recipient’s blood to eventually become Type O.
Also Read - Cost of Bone Marrow Transplant in Government Hospitals
Why Does Graft vs Host Disease Happen?
The donor T-cells attack the recipient’s tissues such as the skin, liver and gut cells. This mainly occurs when the donor immune cells recognize the host cells as “foreign” - leading to a severe reaction.
This disease is an immunological reaction which occurs when the donor’s immune cells recognize the recipient’s healthy cells as the enemy. Because post-transplant the donor’s blood cells start spreading in the recipient’s body, the leftover original recipient cells trigger a immunological reaction.
Some T-cells are desirable in the donor graft as it helps the marrow engraft and to fight any residual cancer cells. When they become too much - it increases the risk of GVHD.
T-cell depletion can reduce the risk but it can increase the risk of graft failure or relapse of cancer.
In addition, some donor characteristics can lead to GVHD risk. For example, an older donor who had previous pregnancies when donating to male recipient can increase the risk of T-cells reacting.
Some of the organs that are affected due to GVHD include the skin, liver, gastrointestinal tract, eyes, joints, lungs and muscles - especially in GVHD.
CMV in Bone Marrow Transplant Patients
Cytomegalovirus or CMV reactivation is a serious complication after BMT which leads to severe illness which affects the survival rates. This is mainly due to the patient’s immunocompromised state.
CMV is a latent herpesvirus that most adults are asymptomatic carriers of - after BMT, the weakened immune system leads to reactivation of the virus.
Those who have undergone allogeneic BMT, are GVHD patients or CMV-seropositive recipients or donors have the highest risk of this .
Other failure symptoms are discussed below.
Also Read - BMT in Government Hospitals of India
Bone Marrow Transplant Failure Symptoms
Recipients experience failure symptoms that must be reported immediately:
BMT failure symptoms for the recipient include:
-
Persistent fever
-
Unexplained weakness and fatigue
-
Severe infections
-
Absence of rising blood counts
-
Paleness of the skin and mucus membranes
-
Requiring continued transfusions
Bone Marrow Transplant Donor Risks
There is no concept of failure for BMT donors, they are at the risk of experiencing side effects such as below:
-
Pain -Donors experience pain at the aspiration site which is usually the back or hip. This is similar in feeling as a strained back or muscle pain.
-
Fatigue: Donors commonly feel tired after the procedure.
-
Bruising: On the bone marrow aspiration site, there can be bruising.
-
Other: Headaches, muscle pain and soreness.
There may be long-term effects such as sexual dysfunction, but this is rare.